Portal, AZ - Rodeo, NM
Serving The Communities Of Portal and Rodeo (www.portal-rodeo.com)
Serving The Communities Of Portal and Rodeo (www.portal-rodeo.com)

Template
Medical Helicopter

LifeLine/Air Evac
When a medical professional determines emergency transport is necessary, they may decide that air ambulance is the fastest and safest way to get you to the care you need.
If requested by a hospital or first responder, AirMedCare Network providers respond with caring, experienced, highly-trained crews and aircraft equipped with the latest life-saving and life-support equipment.
You’re transported to the closest appropriate hospital for continuing care.




MOST FREQUENTLY ASKED QUESTIONS
If I am a member but end up being transported by a ground ambulance or another air ambulance service, who is responsible for the bill?
If an AirMedCare Network Provider does not transport you, you will be responsible for payment. Our membership program only covers transports provided by our affiliates.
Is there a limit to the number of transports a member can have in a year?
There is no limit to the number of transports a member may take in a year. Each transport is handled the same way and must be a life-or-limb-threatening emergency as deemed by AMCN Provider attending medical professionals.
Can I cover all of my family on the membership?
With an AirMedCare Network membership, any person or persons who reside under one (residential) roof are covered. In the event we have a member who lives in a duplex or apartment complex, we designate the primary member’s residence/address— that is considered the “one roof”. Undergraduate college students can be covered under their parent’s membership as well as anyone previously residing in the household who is then moved to a permanent care facility.
I heard that you have a discounted membership for seniors. How old do I need to be in order to qualify?
To ensure coverage remains affordable, we have created a senior pricing option for our primary and/or secondary members who are at least 60 years old.
What is a primary or secondary member?
The primary member is the one in whose name the account is opened. For current member households, we are automatically assigning the person closest in age to the primary member as the secondary member. For new members enrolling online, you can designate the secondary member when adding additional members living in your home to your membership.
I signed up for a membership last year and it’s time for me to renew. I’m 54 years old, but my husband is 60 years old. Do we qualify for the senior discount?
Yes. Your husband can be designated as the secondary member and would qualify your household for our senior pricing option. Please contact our call center to confirm that your husband is listed as the primary or secondary member. If not, they can make this change for you.
What is included in a member’s insurance, other benefits and third party responsibility?
These are all potential sources for payment that can be applied to pay for the transport of any patient, including a member patient, by an AirMedCare Network Provider. Accordingly, any type of insurance- health, auto, medical, liability, etc. – that covers ambulance transport services is included. Any benefit- such as another membership that covers medical services, workers’ compensation benefits, etc. – is included. Any third party who is responsible or liable for paying the cost of medical services, such as an at-fault driver of an automobile or the at-fault person’s liability insurance carrier is also included. Medicare is a secondary payer and requires AirMedCare Network Provider to seek payment from third party liability sources before billing Medicare for patient transports. Many commercial health insurance plans also have rules that, in effect, make third party liability payments primary. Members agree that the AirMedCare Network Provider is entitled to any and all payment received from insurance, benefit providers and/or any third party for air medical services provided by the AirMedCare Network Provider.
If I have Medicare and a supplemental policy, do I need a membership?
The answer varies, depending upon the nature of your transport and your supplemental insurance provider. In many cases, Medicare and the supplemental insurance coverage should pay for the cost of transport if it is medically necessary and if Medicare believes you were taken to the closest appropriate hospital. However, AMCN has seen cases in which the supplemental insurance provider does not cover a remaining balance after Medicare has paid its portion. Many seniors have said they want a membership even if they have complete coverage, in the event that their insurance coverage changes in the future or if the claim is denied. Often time’s supplemental insurance won’t pay if your primary insurance denies. In those circumstances, membership is very beneficial.
My insurance company says they will cover 100% so why do I need this membership?
Most insurance companies will pay 100% of what they deem an allowable amount for air ambulance or emergent ground, which does not necessarily mean that the total cost of the transport will be covered. For example, even after insurance pays, you may have a remaining balance due to co-pay, deductible, co-insurance, or because your insurance’s allowable amount does not cover the total charges. Additionally, people frequently change insurance companies and plan designs. You may want to check with your individual insurance company to find out exactly how much they will cover in the case of an AMCN transport. Lastly, your insurance may decide that the flight does not fit a specific parameter covered under your policy and deny payment. Membership will cover the cost of the flight for you, even if your insurance does not.
Who decides where to fly the patients?
When an air ambulance provider is called, time is of the essence. Patients in life-threatening situations often need specialty centers to provide the interventions needed. AirMedCare Network Providers will take a patient to the closest appropriate medical facility as determined by physicians or EMS personnel. Whenever possible, physicians or EMS personnel consult with the patient or the patient’s families as these decisions are being made.
Does a membership ensure that AirMedCare Network will fly me, no matter what type of medical care I need?
Air ambulances are valuable and scarce resources that should be reserved for those times when a patient is facing a life-or-limb-threatening emergency and it is in their best interest to get to medical care in a timely fashion. AirMedCare Network Providers will not transport patients by air if air transportation is not believed to be appropriate.
Who determines if and when I will be flown?
If your medical emergency meets certain criteria, such as a heart attack, stroke or a traumatic injury, and the 911 dispatcher determines you would benefit from emergent ground or air medical transport, they may dispatch an air ambulance to your emergency, as well as a ground ambulance. If you require an emergent medical transport from one hospital to another hospital, those transfers are ordered by physicians. In the event that the AirMedCare Network Operations Center receives a call for emergency help from an individual or source other than a healthcare or emergency services agency, AirMedCare Network Providers communication specialists will identify and contact the ground EMS service in the patient’s community and ask them to respond to the scene. If they determine air medical transport is needed, they will dispatch one of our air ambulance providers.
________________________________________________________________________
PHI CARES WEB SITE
PHI CARES
BENEFITS OF MEMBERSHIP
There are many reasons for choosing to become a member with one of the world’s most respected and safest air medical organizations.
While none of us ever expect to be in a situation where we or a loved one will need to be transported via an air ambulance, the reality is that it could and does happen. Seconds can make all the difference during a stroke, heart attack, serious car accident, or other trauma. The last thing you should be concerned with during such an emergency is air transportation costs.
That’s why it’s comforting to know that the first air ambulance company to be recognized with the Vision Zero Aviation Safety Award serves your community. When you become a member of the PHI Cares Membership Program, PHI will accept the insurance payment or other third party payment as “payment in full” for any medically necessary transport – from one medical facility to another medical facility, or from the scene of an emergency. As a member, when transported by PHI Air Medical or one of our partners, you will be relieved from any other charges in connection with your air medical transport aboard a PHI Air Medical or one of its partners’ aircraft.
MOST FREQUENTLY ASKED QUESTIONS
Why Should I Become a Member of the PHI Cares Membership Program?
While none of us ever expects to be in a situation where we need to be transported by an air ambulance, the reality is it can and does happen. Time can make all the difference during a stroke, heart attack, serious car accident, or other life-threatening trauma. The last thing you should be concerned with during such an emergency is air transportation costs. As a PHI Cares member, when transported by PHI Air Medical or one of our cooperative service partners, you will never have any out-of-pocket expenses for medically-necessary air transports; PHI Air Medical will work with your insurance provider and accept the insurance payment as “payment-in-full” for any medically-necessary transport – from one medical facility to another medical facility, or from the scene of an emergency. For more details on our program, please visit our website at www.phicares.com
How does the Membership program work?
PHI Air Medical works closely with local fire departments, ground ambulances, law enforcement agencies, medical facilities, and physicians, to ensure safe, expedient, and lifesaving care for our patients. Members should always call 911 when they have a medical emergency. The 911 dispatchers are trained to gather specific information about the medical emergency from the caller and determine what type of medical transportation is best for the situation. If the 911 dispatcher determines the patient requires an air medical transport, they will request an air ambulance. PHI Air Medical specialists are on duty 24 hours a day, 365 days a year, to respond to medical emergencies. Your membership with PHI Cares will help ensure you and your qualified household dependents are covered when they are transported by PHI Air Medical. Members should always ask for PHI Air Medical when possible, especially for hospital transfer flights. We will work with your insurance provider to make sure there are no outstanding out-of-pocket costs for your emergency air medical transport.
How many people does my PHI Cares Household Membership cover?
A household is considered to include all immediate family members and up to three (3) non-family members who reside in the same household on a full-time basis. Members are required to register all dependents and qualified non-family members living at the same address on their membership application or website enrollment portal.
If I’m flown by another air ambulance company, will my membership cover their bill?
Your PHI Cares National Membership provides benefits if PHI Air Medical or one of our cooperative service partners transports you or a qualified household member. PHI has over 60 flight bases across the nation with a helicopter service range up to 200 nautical miles. Your membership does not cover charges from other service provider. For a current map of our service areas and cooperative service providers, please visit the PHI Cares website: www.phicares.com
I have Medicare, do I need to have a PHI Cares Membership?
Medicare does not pay 100% of your medical bills, therefore your PHI Cares membership is ideal for anyone on Medicare and/or a fixed income who might otherwise have to absorb the portion of your air medical transport bill not covered by your insurance or other third party. For just pennies per day, you can have the peace of mind in knowing you and your qualified household dependents are covered in the event of an emergency. We will work with your insurance provider to make sure there are no outstanding out-of-pocket costs for your emergency air medical transport. Medicare participants with supplemental insurance should contact their insurance provider to verify their specific benefits and out-of-pocket expense for emergency air medical transports.
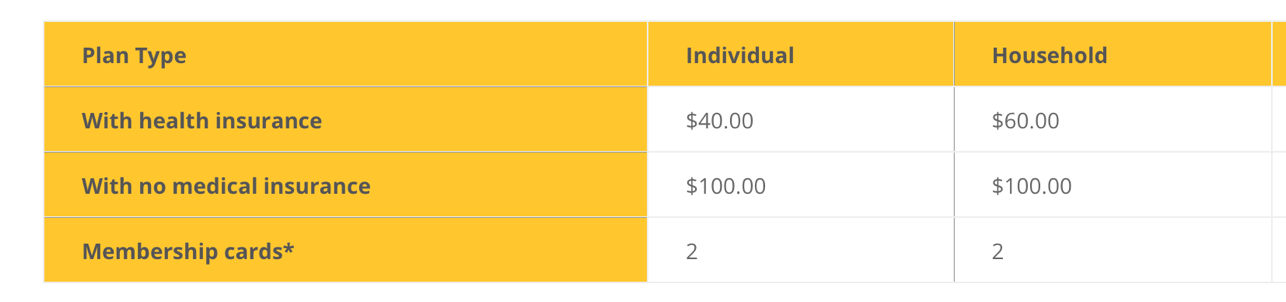
If I don't have medical insurance, can I still sign-up for the membership program?
Health insurance is not required, however the membership rates are $100.00 for an individual or household national membership with no insurance. Please note: Medicaid members are not eligible to enroll in this program*.
What should I do if I have a membership and me or an eligible family member is transported by PHI Air Medical?
You should notify the Membership office if you or an eligible family member is transported by PHI Air Medical. This will help ensure you don’t receive a bill for your transport.
If I’m transported by ground ambulance to the PHI aircraft, will my membership cover the cost of the ground ambulance?
Your PHI Cares membership does not cover ground ambulance charges. Members should contact their insurance companies to verify their specific benefits and out-of-pocket expense for ground ambulance transports.
Is PHI Air Medical guaranteed to be available when requested for a transport?
We cannot guarantee a PHI Air Medical aircraft will be available whenever a member transport is requested. We operate 60 flight bases across the nation, but due to operational and safety factors including, among others, adverse weather, the aircraft is in use at the time of the request, or aircraft maintenance may prevent PHI Air Medical from responding to a request for an air medical transport, so PHI Air Medical and other air medical operators cannot guarantee they will always be available when a member transport is requested. We encourage all members to enroll in all air medical membership programs operating in their area.
At the present time, we are serviced by two competing companies, and we never know which service will show up. A major point of confusion is the necessity of purchasing the plans of the services if you have Medicare. While I do not know anyone who had to shell out tens of thousands of dollars for the helicopter ride, the annual fees are not that high and worth investigating
What Does Medicare Say?
MOST FREQUENTLY ASKED QUESTIONS
What Does Medicare Say?
I have (several times) spoken with a Medicare representative. The question I ask is as follows:
In our small, unincorporated town, we have trained volunteer EMTs that respond to medical emergencies. Douglas Fire department sends out paramedics. Suppose they suspect a patient is having a heart attack and call for the helicopter. At the hospital, the diagnosis is severe indigestion. Not being a life-threatening condition, what would be Medicare’s decision about payment. The rep said there was NO objective answer. Every case is judged on its merits. If there was no physician to make the call and the EMTs decided the person might be having a heart attack, that would be an important factor in the decision. Incidents like this, with all their ramifications and nuances, are not spelled out in any Medicare manual. So, that’s the best we can do. If a claim is denied, it can be appealed.
And it’s not Just Medicare…
ALL insurance companies are going to be judging each case on the merits of hospital tests – tests that aren’t available to EMTs and paramedics in the field.
Reason number 1 to carry helicopter memberships:
A specific medical helicopter company cannot be requested. The closest available company will respond to the emergency.
Reason number 2:
EMTs and paramedics cannot diagnose, they can only treat signs and symptoms. Many “benign” signs and symptoms mimic life-threatening illnesses that can only be diagnosed by a doctor with tests and medical scans available to them. Some of these “benign” illnesses are actually the body’s way of warning people that a more serious illness is likely to happen.
Reason number 3:
Another reason is that we are actually under a protocol that approves medical helicopter transport if a patient is more than one hour from advanced care. That hour actually begins at the time of illness or injury – not when EMTs arrive to assess the situation – not when the person is finally on their way to advanced care.
Reason number 4:
You may not have reached your Medicare or insurance deductible balance. And that company will bill you for that amount. If you have a membership, you will receive a ZERO balance, no matter what amount your insurance company doesn’t cover.
Howeird